Lynch syndrome
Lynch syndrome is a genetic condition that can be passed down in families. It increases a person’s chance of getting bowel cancer and other types of cancer.
Lynch syndrome is linked to around 1 in 30 (3%) cases of bowel cancer. Both men and women with Lynch syndrome have a higher chance of developing bowel cancer. Around 8 in 10 (80%) people with Lynch syndrome will get bowel cancer during their lifetime.
Lynch syndrome also increases the chance of developing womb (endometrial) cancer. It slightly increases the chance of developing of other cancers, including ovarian, stomach and pancreatic cancer.
Diagnosing Lynch syndrome
If you've been diagnosed with bowel cancer, testing for Lynch syndrome usually involves three steps:
1. Screening Tests
All patients diagnosed with bowel cancer should be offered screening tests on their tumour. These tests check how well your DNA repairs itself to prevent cancer. There are two different types of screening tests:
- Mismatch repair (MMR) protein testing – looks at levels of proteins (called MMR proteins) in the tumour
- MSI genetic testing – looks for changes in short sections of DNA called microsatellites
If your tumour has low levels of MMR proteins (called dMMR), or lots of MSI genetic changes (called MSI-H), you may have Lynch syndrome, but another test is needed to confirm it.
It’s useful to write down your screening test results (sometimes called your status), as you may be asked about them in the future.
2. Genetic counselling
If the screening test results suggest you might have Lynch syndrome, you'll be referred to clinical genetics services. They’ll explain genetic testing, what it involves and how the results could affect you and your family. You can then decide whether to go ahead with genetic testing.
3. Genetic testing
If you decide to have a genetic test, it involves a simple blood or saliva test to check for Lynch syndrome.
If you have been diagnosed with womb (endometrial) cancer you should also be tested for Lynch syndrome.
How does Lynch syndrome cause cancer?
Every cell in your body contains genes that act like instructions, to keep you healthy. If a gene is changed, the instructions may not be correct and the body may act differently. A gene change can also be called a variant, mutation, gene fault or gene error.
Mismatch repair genes help protect the body from cancer. In people with Lynch syndrome, these genes do not work properly, which means cancer is more likely to develop.
Lynch syndrome is caused by a gene change in a group of genes called Mismatch Repair genes. The mismatch repair genes include: MLH1, MSH2, MSH6 and PMS2. Lynch syndrome can also be caused by changes in the EPCAM gene, but this is less common. Your genetic test results will show which gene is affected and this may influence monitoring and treatment options.
Inheritance
Lynch syndrome is caused by a change in one of the mismatch repair (MMR) genes or the EPCAM gene.
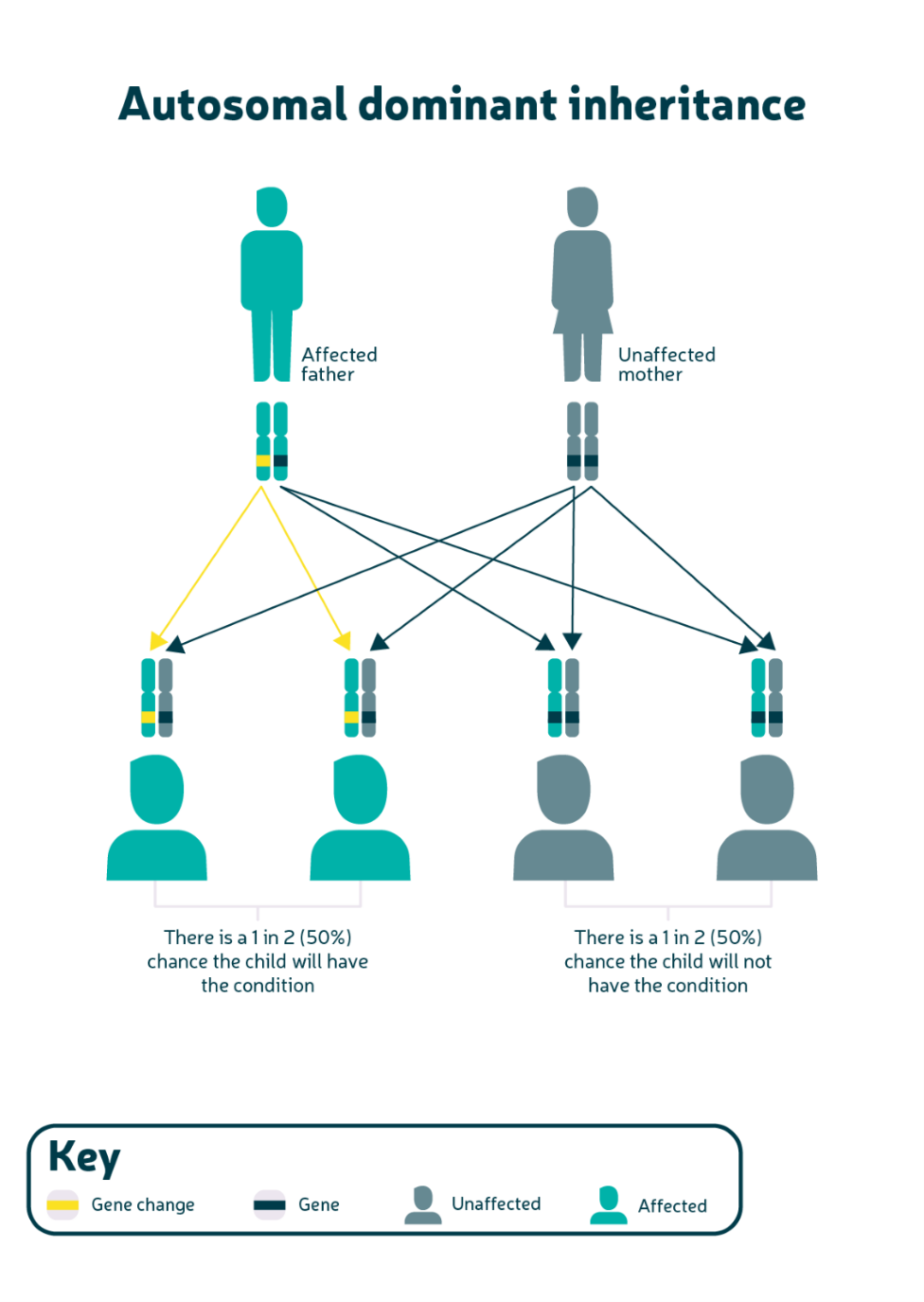
Only one copy of the changed gene needs to be passed on (inherited) for a person to have Lynch syndrome.This is called autosomal dominant inheritance (see diagram below). If you have Lynch syndrome, there’s a 1 in 2 (50%) chance that your children, full siblings and parents also have it too.
Tell your doctor if you have a relative with Lynch syndrome or a family history of bowel cancer and/or womb (endometrial) cancer.
If you’re planning to have children, you may have questions about the risk to your children. Your genetics team will be able to answer these. They'll also be able to discuss other fertility options with you. The Human Fertilisation and Embryology Authority have more information about options available to you.
Reducing your chance of developing bowel cancer
If you have Lynch syndrome, you can access check-ups and screening tests to help catch cancer early. You'll also receive advice about lifestyle changes that can reduce your chance of getting cancer.
People a with Lynch syndrome are offered a colonoscopy every two years to catch cancer early when it’s most treatable and curable. The age at which you start colonoscopies depends on the gene change you have.
For MLH1, MSH2 and EPCAM gene changes: it's recommended that these patients have a colonoscopy every two years from the age of 25 to 75 years old.
For MSH6 and PMS2 gene changes: it's recommended that these patients have a colonoscopy every two years from the age of 35 to 75 years old.
These starting ages vary because each gene change increases the chance of developing cancer by different amounts.
The helping you decide leaflet provides more information about bowel screening if you have Lynch syndrome. The leaflet is also available in Easy Read format.
You may be advised to take daily aspirin, which reduces the chance of getting bowel cancer for people with Lynch syndrome.
Other ways to reduce your chance
You may be advised to take daily aspirin, which reduces the chance of getting bowel cancer for people with Lynch syndrome.
Other ways to reduce your chance include:
- Increasing the amount of fibre in your diet
- Avoiding eating processed meats
- Avoiding drinking alcohol
- Reducing the amount of red meat in your diet
- Being a healthy weight
- Being physically active
- Not smoking
Our ‘Simple steps to good bowel health’ booklet has more information about reducing your chance of developing bowel cancer.
If you have Lynch syndrome, you may have surgery to remove part or all of the large bowel. Women, trans men and other people assigned female at birth with Lynch syndrome may also be offered surgery to remove the uterus (hysterectomy) and ovaries (oophorectomy) at the same time. This is to avoid the chance of developing womb (endometrial) and ovarian cancer. After surgery, you’ll have regular colonoscopies to monitor the remaining colon.
The Lynch Choices website provides information to help you make decisions around having Lynch syndrome, such as taking aspirin and having surgery.
If you have Lynch syndrome, you may want to ask your healthcare team:
- Which gene change do I have?
- Should I take aspirin?
- When is my next screening appointment?
If you have been diagnosed with bowel cancer but not tested for Lynch syndrome, you should speak to your healthcare team who can refer you to clinical genetics. Bring as much information as you know about your family history. If possible, try to include:
- any family members diagnosed with cancer
- the type of cancer they were diagnosed with
- the age they were diagnosed at
What about my family?
If you’ve been diagnosed with Lynch syndrome, there is a 50% chance that your children and siblings also having the condition. Your family members may choose to have genetic testing. You can speak to your doctor about having your family screened for Lynch syndrome if you’ve been diagnosed with it.
All family members should tell their GP if they have:
- a close relative (parent, sibling or child) diagnosed with bowel cancer before the age of 50 years
- two or more close relatives diagnosed with bowel cancer at any age (for example your parent, and their sibling or parent)
- a relative with a known genetic (inherited) condition linked to bowel cancer, such as Lynch syndrome or familial polyposis
If any of your family members are diagnosed with Lynch syndrome, they’ll be offered a colonoscopy every two years as part of the bowel cancer screening programme. They’ll start from the age of 25 or 35, depending on the gene change found. This allows any growths (polyps) to be removed and cancer to be picked up early. They might be offered other options to reduce their chance of getting bowel cancer, such as taking aspirin, making lifestyle changes or having surgery to remove part of the colon (colectomy). Ask your healthcare team for more information on what screening is available. If your relatives don’t want to have a genetic test, they can still have regular screening if they have a 1 in 2 (50%) chance of carrying the gene change.
More information
If you have questions after being diagnosed with Lynch syndrome, your healthcare team should be able to help answer them.
Lynch syndrome UK provide information and support for people with Lynch syndrome. They also have an online support group with over 2000 other people with Lynch syndrome.
The Lynch Syndrome UK app provides a summary of the condition and has symptom checkers. It can be used by patients, doctors and their relatives. It also signposts to other information and support. The app can be downloaded on Apple and Android.
The Royal Marsden website has a useful beginner’s guide to Lynch syndrome.
The Eve Appeal have a guide to Lynch syndrome which is also available in Easy Read.
Living with Lynch have informative videos featuring people with Lynch syndrome discussing different topics.
The Human Fertilisation & Embryology Authority website has information on costs and funding of fertility treatment and how to choose a fertility clinic.
RM partners have lots of Lynch syndrome information booklets, including advice for speaking to family and children about your diagnosis.
More support
The Peaches Trust provide information for people with, or have a higher risk of womb (endometrial) cancer.
The Eve Appeal provide information and support for people with gynaecological cancers including womb and ovarian cancer.
Our Lynch syndrome campaign
We're campaigning to improve the diagnosis and care of people with Lynch syndrome, a genetic condition that can increase the lifetime risk of bowel cancer to up to 80%. Lynch syndrome is estimated to cause around 3% of bowel cancer cases in the UK every year, many of them under the age of 50.
Research
Early diagnosis is a central goal in our research strategy and making sure people with Lynch syndrome are identified and given proper surveillance is an important part of that.
We funded a team at Newcastle University to establish a national Lynch syndrome registry for England by linking together information from the national cancer registration system and genetic testing labs.
We’ve also funded researchers at the University of Birmingham to develop a new way to diagnose genetic risk conditions like Lynch syndrome
Updated: September 2025
Next review: September 2028

We're accredited as a Trusted Information Creator by the Patient Information Forum. This means the way we write our resources has been independently assessed as health information you can trust.
